Enhancing Tracheostomy Weaning with One-Way Speaking Valves
Tracheostomy tube weaning involves gradually reducing dependency on the tube with the goal of removal. This process requires a multidisciplinary approach, potential tube adjustments (like downsizing), and the use of devices such as one-way valves (OWVs).1
Starting ventilator and tracheostomy weaning early and in parallel improves patients' quality of life by enabling partial oral communication and beginning swallowing training.1-4


Laryngeal Rehabilitation: Restoring Swallowing with Tracheostomy Cuff Deflation
A tracheostomy tube with inflated cuff, essential for ventilation, blocks airflow through the upper airways simultaneously. The missing airflow can impair sensory function and affect coughing and swallowing which can lead to complications like dysphagia and aspiration. At the same time, the use of a cuffed tube is indicated for these complications.3,4
Redirecting airflow through the trachea, larynx, and pharynx is crucial for restoring sensation and spontaneous swallowing. Laryngeal rehabilitation, involving cuff deflation and a one-way speaking valve, helps stimulate sensation, improve swallowing, manage secretions, and enable communication.3,4
This process of ‘laryngeal weaning’ is an essential component of the patient’s readiness for decannulation once they are liberated from mechanical ventilation.5
Initiating Verbal Communication with a One-Way Speaking Valve
The inflated cuff of a tracheostomy tube blocks airflow over the vocal cords, causing loss of voice and impacting communication.6 Improved airflow to the upper airway can aid in tube weaning, phonation, reduce respiratory infections, enhance swallowing, and manage secretions better.7-9 However, patients may need time to adapt to the resistance of a one-way speaking valve, which can cause fatigue.1,10

Improving Patient Outcomes with One-Way Speaking Valves
The benefits of using one-way speaking valves create a supportive environment for rehabilitating the laryngeal complex, with a focus on restoring laryngeal airflow and function. This process of "laryngeal weaning" is crucial for preparing the patient for decannulation once they are liberated from mechanical ventilation.5
For further information for Health Care Professionals and Patients download these brochures:
Introducing the Freevent DualCare
Discover Freevent DualCare, a combination of a one-way valve and a Heat and Moisture Exchanger (HME). This device allows patients with a tracheostomy to voice without using their fingers and supports pulmonary rehabilitation by conserving heat and moisture during breathing. Watch the video to learn how easy it is to switch between speaking and breathing modes.

Log in or register to access the step-by-step instructional video on how to use Phon Assist and DualCare. Additionally, you can download a one-page guide to provide a reference in clinical practice.
Download step-by-step guide on how to use Tracoe Phon Assist.
Download step-by-step guide on how to use DualCare.

Managing Swallowing Dysfunction and Secretion Control
Swallowing dysfunction affects 30% to 70% of tracheostomy patients due to the close link between breathing and swallowing.11 Clinicians use various strategies, for instance downsizing of the cannula, to optimize airflow to the upper airway, improving swallowing, secretion clearance, coughing, and airway protection.12 Early cuff deflation and using a one-way speaking valve can help reduce aspiration during swallowing.8
Normalizing Upper Airway Physiology Benefits Health and Senses
- Restores PEEP: Re-establishes the ability to generate physiological Positive End Expiratory Pressure (PEEP) from the upper airway5,8
- Subglottic Pressure: Enables the generation of subglottic pressure, which enhances the success of swallowing and reduces the risk of aspiration5,8
- Glottic Closure: Supports glottic closure, necessary for an effective cough and airway protection, by triggering the laryngeal adductor reflex5,8
- Sensory Stimulation: Enhances laryngopharyngeal sensory stimulation, improving awareness of pooled saliva secretions and the need to swallow5,8
- Taste and Smell: Improves the senses of taste and smell5,8
Pulmonary Health in Tracheostomy Weaning
Pulmonary health is crucial in tracheostomy weaning. The upper airways naturally humidify and filter air, but a tracheostomy bypasses these functions, allowing unconditioned air and particles to enter the lower airways, potentially causing issues like excessive mucus and coughing.13,14
Exploring the Standards in Humidification
Patients with a tracheostomy face challenges in maintaining optimal lung and tracheal climate due to the absence of natural heat and humidification from the upper airways. While active humidification is common in hospital settings, passive humidifiers like Heat and Moisture Exchangers (HMEs) offer a portable and effective alternative. This Whitepaper reviews research on HMEs and user feedback on the TrachPhone device, highlighting positive outcomes and future research directions.

Heat Moisture Exchangers: Boosting Respiratory Comfort and Function
Heat and Moisture Exchangers (HMEs) help retain heat and moisture during exhalation and return them during inhalation. Using HMEs can improve air humidity and temperature, reduce mucus viscosity, lessen coughing, and enhance respiratory function.14
They may support patient mobility, rehabilitation, compliance, and comfort more effectively than external humidifiers.15 HMEs can reduce adverse events like mucus plugs and the need for chest physiotherapy.16 To maximize humidification, an HME should be used when a one-way speaking valve is not in use, either through a combined device or a separate HME.
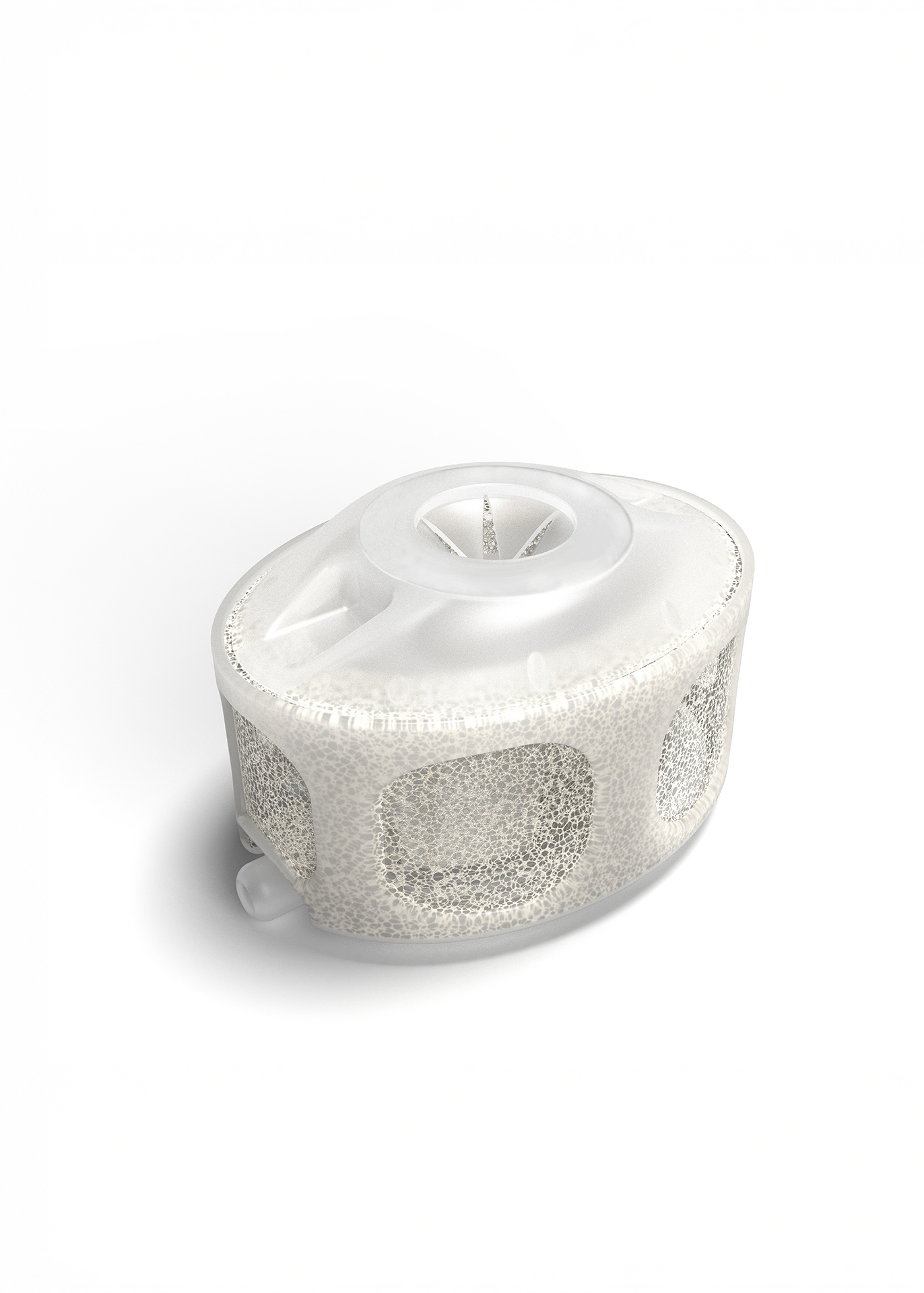
TrachPhone
An HME offering effective pulmonary and vocal rehabilitation for tracheostomy patients
For further information for Health Care Professionals and Patients download these brochures:
Explore our solutions:
Tracoe Phon Assist I, TrachPhone and Freevent DualCare
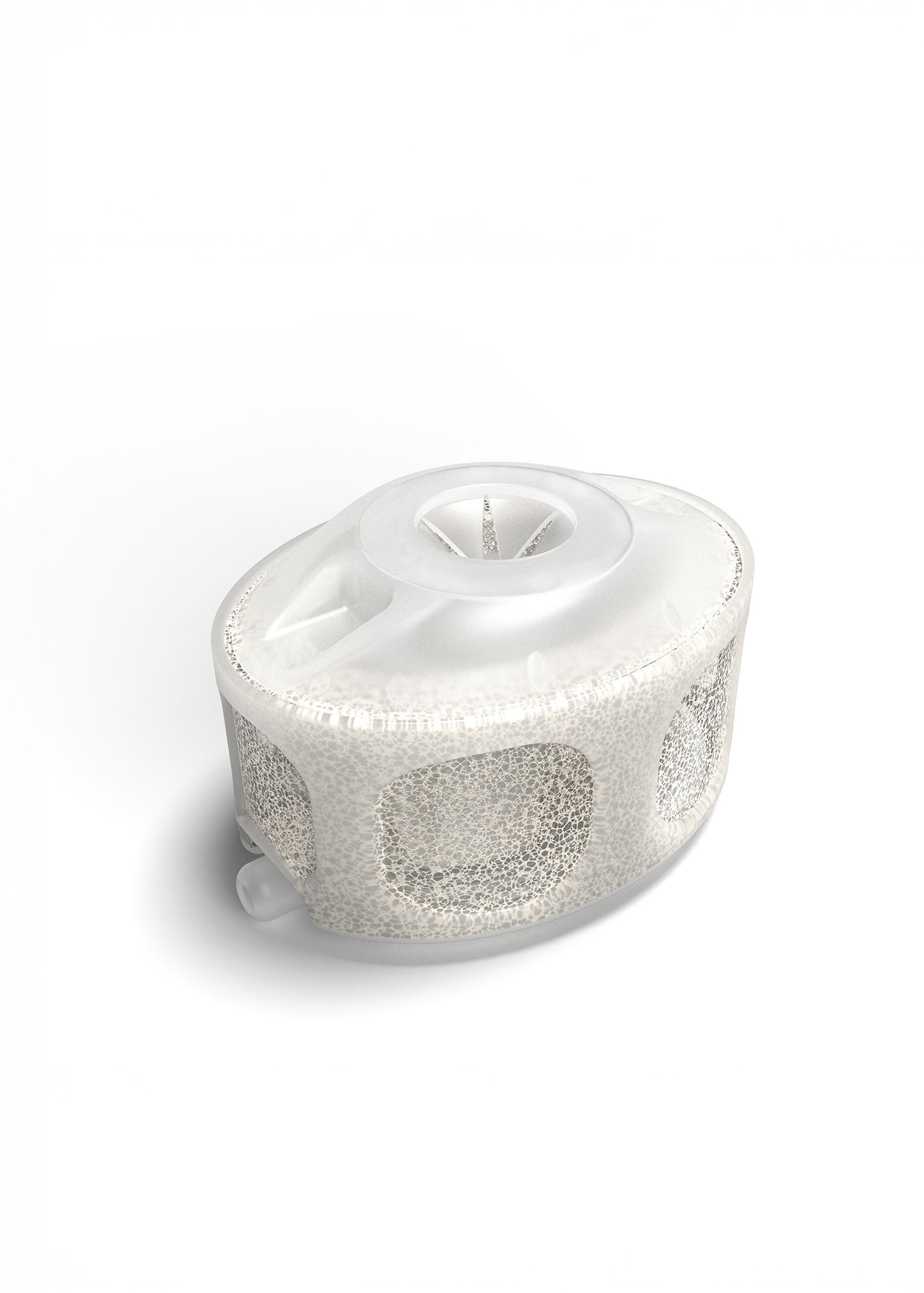
TrachPhone
An HME offering effective pulmonary and vocal rehabilitation for tracheostomy patients
References
1. Hunt K, McGowan S. Tracheostomy management. BJA Education. 2015 Jun 1;15(3):149-53.
2. Pham T, Heunks L, Bellani G, Madotto F, Aragao I, Beduneau G, Goligher EC, Grasselli G, Laake JH, Mancebo J, Peñuelas O. Weaning from mechanical ventilation in intensive care units across 50 countries (WEAN SAFE): a multicentre, prospective, observational cohort study. The Lancet Respiratory Medicine. 2023 May 1;11(5):465-76.
3. Schwegler H. Trachealkanülenmanagement. 4th edition. Idstein: Schulz-Kirchner Verlag GmbH; 2022. p. 1-208.
4. Heidler MD, Salzwedel A, Jöbges M, Lück O, Dohle C, Seifert M, et al. Decannulation of tracheotomized patients after long-term mechanical ventilation – results of a prospective multicentric study in German neurological early rehabilitation hospitals. BMC Anesthesiology. 2018 Jun 13;18(1).
5. Wallace S, McGowan S, Sutt AL. Benefits and options for voice restoration in mechanically ventilated intensive care unit patients with a tracheostomy. J Intensive Care Soc. 2023 Feb;24(1):104-111.
6. Sutt AL, Caruana LR, Dunster KR, Cornwell PL, Anstey CM, Fraser JF. Speaking valves in tracheostomised ICU patients weaning off mechanical ventilation-do they facilitate lung recruitment?. Critical Care. 2016 Dec;20:1-9.
7. Hernandez G, Pedrosa A, Ortiz R, Cruz Accuaroni MD, Cuena R, Vaquero Collado C, García Plaza S, González Arenas P, Fernandez R. The effects of increasing effective airway diameter on weaning from mechanical ventilation in tracheostomized patients: a randomized controlled trial. Intensive Care Medicine. 2013 Jun;39:1063-70.
8. Rose L, Messer B. Prolonged Mechanical Ventilation, Weaning, and the Role of Tracheostomy. Critical Care Clinics. 2024 Apr 1;40(2):409-27.
9. O’Connor LR, Morris NR, Paratz J. Physiological and clinical outcomes associated with use of one-way speaking valves on tracheostomised patients: A systematic review. Heart & Lung. 2019 Jul;48(4):356–64.
10. Prigent H, Orlikowski D, Blumen MB, Leroux K, Legrand L, Lejaille M, Falaize L, Ruquet M, Raphael JC, Lofaso F. Characteristics of tracheostomy phonation valves. European Respiratory Journal. 2006 May 1;27(5):992-6
11. Whitmore KA, Townsend SC, Laupland KB. Management of tracheostomies in the intensive care unit: a scoping review. BMJ open respiratory research. 2020 Jul 1;7(1):e000651.
12. Skoretz SA, Anger N, Wellman L, Takai O, Empey A. A systematic review of tracheostomy modifications and swallowing in adults. Dysphagia. 2020 Dec;35:935-47.
13. Wong CY, Shakir AA, Farboud A, Whittet HB. Active versus passive humidification for self‐ventilating tracheostomy and laryngectomy patients: a systematic review of the literature. Clinical Otolaryngology. 2016 Dec;41(6):646-51.
14. van den Boer C, Lansaat L, Muller SH, van den Brekel MW, Hilgers FJ. Comparative ex vivo study on humidifying function of three speaking valves with integrated heat and moisture exchanger for tracheotomised patients. Clin Otolaryngol. 2015 Dec;40(6):616-21.
15. Mérol JC, Charpiot A, Langagne T, Hémar P, Ackerstaff AH, Hilgers FJ. Randomized controlled trial on postoperative pulmonary humidification after total laryngectomy: external humidifier versus heat and moisture exchanger. The Laryngoscope. 2012 Feb;122(2):275-81.
16. Foreman A, De Santis RJ, Sultanov F, Enepekides DJ, Higgins KM. Heat and moisture exchanger use reduces in-hospital complications following total laryngectomy: a case-control study. J Otolaryngol Head Neck Surg. 2016 Jul 7;45(1):40.
MC3307-TcEn202411

