Above Cuff Vocalization (ACV): Improving Communication for ICU Patients with Tracheostomy
In the ICU, patients on invasive mechanical ventilation often face communication barriers due to the inflated tracheostomy tube cuff. This cuff, while medically necessary, prevents air from flowing through the larynx and vocal cords, making speech impossible and reducing oropharyngeal sensitivity, which affects swallowing and coughing abilities. Above Cuff Vocalization emerges as a promising method to address this challenge.1-3

Interview
Meet Sarah Wallace: Inspiring SLT Leader
Get to know Sarah Wallace and her inspiring experiences and learn about the benefits of ACV for ventilated patients.
Sarah Wallace is a Consultant Speech and Language Therapist at Manchester University NHS Foundation Trust (MFT). In addition to her frontline role in MFT Critical Care, based at Wythenshawe Hospital, Sarah is SLT lead for the National Tracheostomy Safety Project and the Intensive Care Society (ICS); and a Specialist Advisor in Critical Care and Dysphagia for the Royal College of Speech and Language Therapists (RCSLT).
The Impact of ACV on Quality of Life in Tracheostomized Patients
Above Cuff Vocalization (ACV) has shown promising results in improving communication for tracheostomized ICU patients, with around 50 to 80% achieving vocalization when cuff deflation is not possible.1-3,8 Studies, including a randomized controlled trial, highlight ACV's safety and benefits, such as successful phonation, enhanced cough and swallow function, and improved quality of life.2-4

Deb's journey with ACV
Witness Deb's remarkable journey with the help of ACV. See how improved communication has transformed her and her husband Mike's lives, bringing them more comfort and confidence. Discover the power of a voice and the difference it makes in healing and connection.

The Impact of Subglottic Suction Tubes
Subglottic suction tracheostomy tubes are increasingly used in acute settings to reduce ventilator-associated pneumonia (VAP) and mortality.5-7 These tubes also enable earlier application of Above Cuff Vocalization (ACV)8, addressing both medical and communication needs. This dual approach ensures effective secretion management and allows patients to vocalize, improving their mental and physical well-being.4
Benefits of Above Cuff Vocalization (ACV)
- Enhanced Communication: ACV allows patients to speak, significantly improving their ability to communicate with healthcare professionals and family members, which can reduce anxiety, stress, and depression.1-4
- Improved Laryngeal Function: By enabling vocalization, ACV can help maintain and rehabilitate laryngeal function, which is crucial for swallowing and coughing.2,9
- Better Patient Experience: Being able to speak can greatly enhance the overall ICU experience for patients, making them feel more in control and connected.2,4,9
- Potential for Earlier Rehabilitation: Effective communication can facilitate earlier and more effective rehabilitation, contributing to better overall recovery outcomes.2,4,8
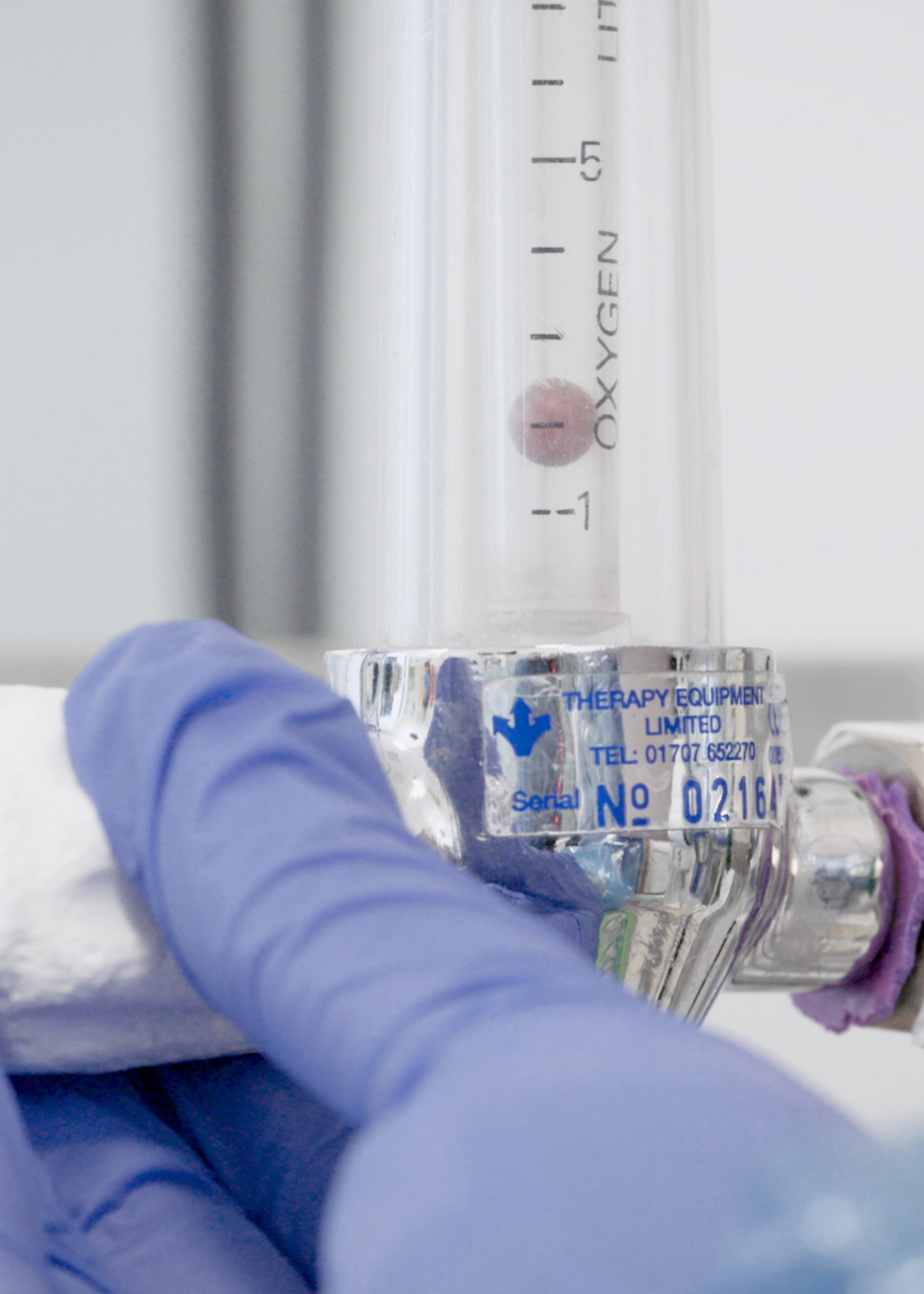
The ACV procedure
Above Cuff Vocalization involves the controlled application of a continuous or intermittent airflow directed through the subglottic port of a tracheostomy tube. This airflow traverses the laryngeal anatomy, allowing for vocalization and the potential restoration of oropharyngeal and laryngeal sensation.
Log in or register to access the step-by-step instructional video, guiding you through the application of ACV in ventilated patients. Additionally, you can download a one-page step-by-step guide to provide a reference in clinical practice as well as some Saftey Guidelines.
Download a one-page guide to provide a reference in clinical practice.
Tracoe Extract Tubes for ACV
All Tracoe Extract tracheostomy tubes are also approved for utilizing the subglottic suction channel or suction line for Above Cuff Vocalization (ACV). To enable voicing, air and/or oxygen can be introduced through the subglottic suction, directed toward the upper airway through the vocal folds.
Always consult the products IFU before initiating ACV to ensure alignment with specific instructions for patient selection and delivery.
Tracoe Twist Extract
Tracheostomy tube with low pressure cuff and subglottic suction
Tracoe Twist Extract
Tracoe Twist Plus Extract
Tracheostomy tube with low pressure cuff and subglottic suction channel
Tracoe Twist Plus Extract
Tracoe Vario Extract
Tracheostomy tube with adjustable neck flange, low-pressure cuff, subglottic suction, scale and 15 mm connector
Tracoe Vario Extract
Learn more about Above Cuff Vocalization:
References
1 Petosic A, Viravong MF, Martin AM, Nilsen CB, Olafsen K, Berntzen H. Above cuff vocalisation (ACV): A scoping review. Acta Anaesthesiol Scand. 2021 Jan;65(1):15-25. doi: 10.1111/aas.13706. Epub 2020 Nov 1. PMID: 32920849; PMCID: PMC7756796.
2 Mills CS, Michou E, King N, Bellamy MC, Siddle HJ, Brennan CA, Bojke C. Evidence for Above Cuff Vocalization in Patients With a Tracheostomy: A Systematic Review. Laryngoscope. 2022 Mar;132(3):600-611. doi: 10.1002/lary.29591. Epub 2021 May 1. PMID: 33932229.
3 McGrath BA, Wallace S, Wilson M, Nicholson L, Felton T, Bowyer C, Bentley AM. Safety and feasibility of above cuff vocalisation for ventilator-dependant patients with tracheostomies. J Intensive Care Soc. 2019 Feb;20(1):59-65. doi: 10.1177/1751143718767055. Epub 2018 Mar 28. PMID: 30792764; PMCID: PMC6376581.
4 Pandian V, Cole T, Kilonsky D, Holden K, Feller-Kopman DJ, Brower R, Mirski M. Voice-Related Quality of Life Increases With a Talking Tracheostomy Tube: A Randomized Controlled Trial. Laryngoscope. 2020 May;130(5):1249-1255. doi: 10.1002/lary.28211. Epub 2019 Aug 6. PMID: 31385620.
5 Pozuelo-Carrascosa DP, Herráiz-Adillo Á, Alvarez-Bueno C, Añón JM, Martínez-Vizcaíno V, Cavero-Redondo I. Subglottic secretion drainage for preventing ventilator-associated pneumonia: an overview of systematic reviews and an updated meta-analysis. Eur Respir Rev. 2020 Feb 12;29(155):190107. doi: 10.1183/16000617.0107-2019. Erratum in: Eur Respir Rev. 2022 Mar 23;31(163): Erratum in: Eur Respir Rev. 2022 Mar 23;31(163): PMID: 32051169; PMCID: PMC9488747.
6 Papazian L, Klompas M, Luyt CE. Ventilator-associated pneumonia in adults: a narrative review. Intensive Care Med. 2020 May;46(5):888-906. doi: 10.1007/s00134-020-05980-0. Epub 2020 Mar 10. PMID: 32157357; PMCID: PMC7095206.
7 Suger-Wiedeck H, Unertl K, von Baum H. Prävention der nosokomialen beatmungsassoziierten Pneumonie. Empfehlung der Kommission für Krankenhaushygiene und Infektionsprävention (KRINKO) beim Robert Koch-Institut [Prevention of nosocomial ventilator-associated pneumonia. The Commission for Hospital Hygiene and Infection Prevention (KRINKO) at the Robert Koch Institute]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013 Nov;56(11):1578-90. German. PMID: 24344412.
8 Gajic S, Jacobs L, Gellentien C, Dubin RM, Ma K. Implementation of Above-Cuff Vocalization After Tracheostomy Is Feasible and Associated With Earlier Speech. Am J Speech Lang Pathol. 2024 Jan 3;33(1):51-56. doi: 10.1044/2023_AJSLP-23-00184. Epub 2023 Dec 6. PMID: 38056485.
9 Wallace S, McGowan S, Sutt AL. Benefits and options for voice restoration in mechanically ventilated intensive care unit patients with a tracheostomy. J Intensive Care Soc. 2023 Feb;24(1):104-111. doi: 10.1177/17511437221113162. Epub 2022 Jul 10. PMID: 36874291; PMCID: PMC9975806.
MC3303-TcEN202410